Why autonomous coding is having a moment in healthcare

Automating medical coding using Artificial Intelligence (AI) has been in the works for more than ten years. As the medical industry got ready for the massive shift from ICD-9 to ICD-10, Health Information Management (HIM) departments needed to adopt automation to assist in the transition without affecting their bottom line.
Over time, as AI developed, so did deep learning and the moment the generative AI models were developed. We’re in the next phase of substantial technological advancements to automate programming workflow fully. The focus is on tackling the shortage of coders and budgetary challenges, which have increased during the last five years. Enter autonomous coding.
What is the real meaning of autonomous coding?
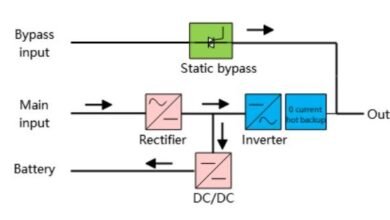
Autonomous medical coding refers to the capability to process digital patient information (e.g., an electronic chart or notes from an experience) and create a reliable finalized code set prepared for the next step during the billing process without human involvement.
Autonomous Coding solutions usually use AI or other logic to produce codes regularly and then mark an encounter as “final coded ready” without human involvement. Therefore, human beings are removed from the interaction with the chart or the documentation of the experience that has passed through the process.
The potential of autonomous code to improve revenue cycle
About the use of self-coding, There are many advantages:
- It eliminates the possibility of human-induced errors, which lead to missing claims, delays, claims mistakes, and backlogs.
- Helps coders to transition into auditors.
- It is aware of what it is unaware of and alerts these charts for human review.
- Completes charts in seconds, and the entire process takes hours.
- Increases the accuracy to near-perfect levels of accuracy.
The trend toward autonomous programming
Medical claims ensure medical coding accuracy and are processed quickly and without revisions. Patients can receive the treatment they require at the time and the proper place for their care. Also, it protects an institution’s financial well-being, which enhances its capacity to provide top-quality health care.
The increasingly complicated nature of coding has resulted in substantial growth in denials due to code and revenue leakage. While nearly two-thirds of claims rejected due to mistakes in medical code or other questions are reversible, the cost of reprocessing claims, the reconciliation, and the payment process often becomes an enormous expense in terms of resources and money. This means that nearly 65 percent of rejected claims never get reworked.
Coding that AI powers are called automated or autonomous coders, helping healthcare revenue cycle professionals manage the complex world of medical Coding. This solution uses machine learning (ML) and natural language processing (NLP) for code assignment, leading to lower claims and less loss of revenue for hospitals and healthcare facilities.
Suppose a look at the claim shows the need for manual intervention, typically for only a small portion of claims. This technology connects the coders to certain types of charts based on their expertise level and areas of experience.
Conclusion
Autonomous medical codes improve the accuracy of claims, decrease denials, and simplify revenue cycles. However, human knowledge is essential for handling complicated cases while ensuring compliance and developing AI-driven coding methods to achieve maximum efficiency in healthcare.